A sticky way to find new drugs – hijacking a danger response in Pseudomonas aeruginosa to reveal novel antimicrobial compounds
A central focus of many researchers in the Institute for Infectious Diseases Research (IIDR) at McMaster University is the search for new drugs or new drug targets to help combat the increasing rise of antibiotic-resistant bacteria worldwide. This aim is being approached in innovative ways by many labs with support from the new David Braley Centre for Antibiotic Discovery. Approaches include looking for compounds that are antimicrobial in infection-relevant conditions, looking for drugs that don’t actually kill the microbe but restrict their virulence potential, and screening for small molecule “potentiators” that improve antimicrobial activity.
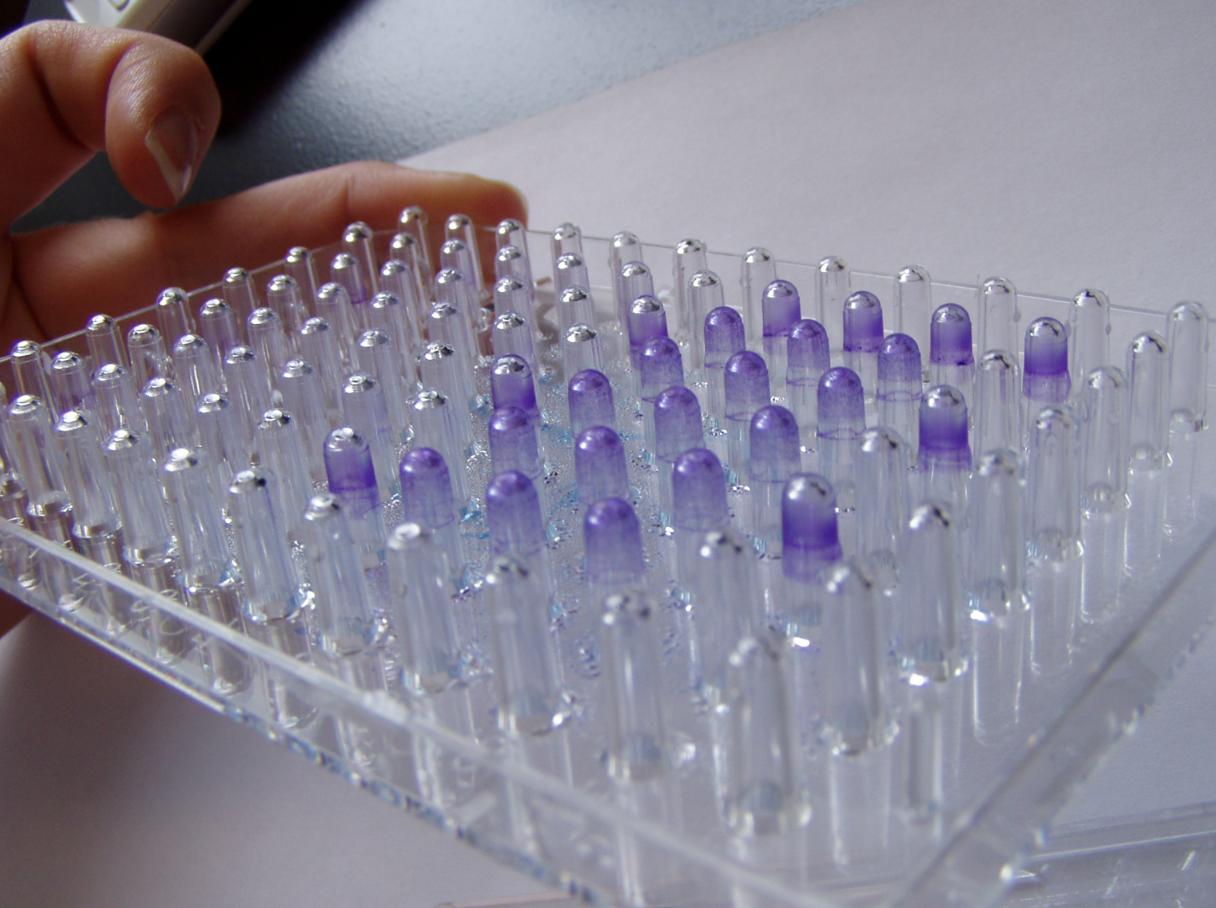
Research led by Biochemistry and Biomedical Sciences professor Dr. Lori Burrows uses this third approach to identify novel anti-virulence compounds against Pseudomonas aeruginosa, an opportunistic pathogen that can cause a variety of infections in immunocompromised humans. Dr. Burrows, who is also the Associate Director of Partnerships and Outreach for the IIDR, wanted to find small molecules that inhibit a particular lifestyle of Pseudomonas that is associated with its ability to cause infections – the formation of biofilms. Biofilms are aggregates of bacteria that attach to a surface and stick onto it through the production of a complex matrix of sugars, proteins, and DNA. Biofilms form on a number of surfaces including medical equipment, which can result in chronic infections, or within the human lung, where they can increase the severity of disease in cystic fibrosis patients. Pseudomonas biofilms are also more resistant to antibiotics, making these infections challenging to treat. To tackle Pseudomonas in this state, Dr. Burrows and her team aimed to probe the ability of a library of previously-approved small molecules to restrict biofilm formation. This screen was initiated by Iwona Wenderska and further developed by Michael Ranieri, both of whom received their Master’s degrees from the Burrows lab. They tested the ability of compounds to limit biofilm formation by measuring the extent of Pseudomonas sticking to a plastic surface following exposure to each compound. Unexpectedly, in addition to finding drugs that restrict biofilms, the students in the Burrows lab found something much more strange – an increase in biofilm formation following exposure to many of these drugs. Sixty compounds in this library caused this phenotype in Pseudomonas, resulting in increased sticking of Pseudomonas to the plastic pegs.
Further examination of this biofilm-stimulating phenotype revealed that many traditional antibiotics and other anti-bacterial molecules, including soaps, had a similar impact on Pseudomonas at sub-inhibitory concentrations. This suggested that biofilm stimulation could be used as a proxy for the detection of potentially toxic molecules. Thus, it appeared that the Burrows group, while searching for biofilm inhibitors, had also uncovered compounds that were previously unknown to have anti-bacterial activity but which behaved like antibiotics in this screen, in that they triggered the same “danger” warning response in Pseudomonas. Indeed, investigation of one of these biofilm-stimulating compounds revealed that it was able to restrict Pseudomonas growth in minimal media and in mouse and human serum, suggesting that it can be used as an anti-Pseudomonas antibiotic during infections. This compound, thiostrepton, has not been previously reported to be anti-microbial against Gram-negative bacteria such as Pseudomonas but was still able to stimulate the Pseudomonas “danger” response and promote biofilm formation, the first clue that it might have anti-Pseudomonas activity. This exciting finding is currently in revision at Antimicrobial Agents and Chemotherapy.
Although a useful way to test massive compound libraries, high-throughput screens for anti-microbial drugs often have low success rates because all the compounds are tested at a single fixed concentration at which the drug might not be effective or potent. Instead of using bacterial killing as a read-out, relying on the bacteria to convey that a compound is potentially harmful by triggering a danger response like biofilm formation allows a large library to be narrowed down to a smaller list of potential compounds that can then be tested for anti-bacterial activity at different concentrations or in different conditions. Although the mechanistic details behind this phenotype are still being characterized by students in the Burrows lab, this novel screening approach is being harnessed by Dr. Burrows’ trainees Derek Chan, Luke Yaeger, and Victoria Coles to identify older drugs that can be repurposed to work against P. aeruginosa. Dr. Burrows and her team hope that this biofilm screen will promote the rapid application of previously FDA approved compounds against Pseudomonas infections in the clinic.
NewsRelated News
News Listing

IIDR News ➚
Fungi in Canada: McMaster researchers survey six provinces, one territory to study trends in environmental fungi
News
November 28, 2024
Faculty of Health Sciences ➚
McMaster researchers get federal funding to study emerging bird flu threat
News
November 20, 2024

Brighter World ➚
Putting the ‘ant’ in antibiotic discovery: How insects could be the key to fighting superbugs
News
November 19, 2024

