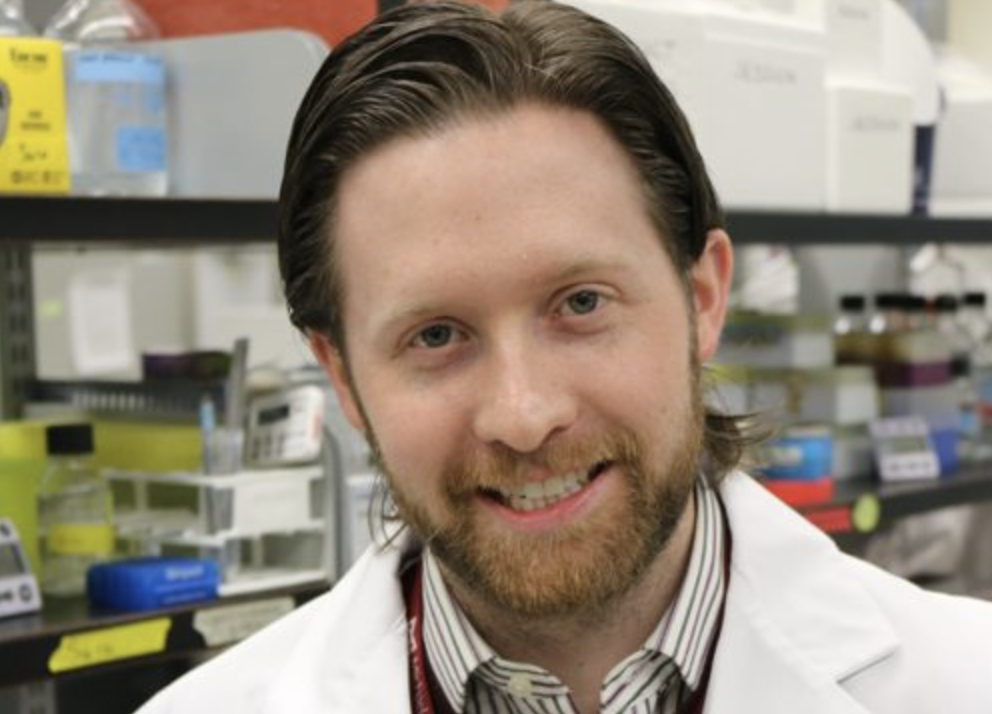
Flu season has begun, and the best line of defense may be this year’s flu vaccine. Dr. Matthew Miller, an assistant professor in the Department of Biochemistry and Biomedical Sciences, and a member of the Michael G. DeGroote Institute for Infectious Disease Research, answers some of the more common questions surrounding the virus and its vaccine.
What is the influenza virus?
“There are two types of influenza viruses that can lead to seasonal epidemics in the fall and winter months. These are influenza A and B. However, in terms of potential risk, the influenza A virus – commonly referred to as the ‘flu’ – is the most serious. Every year since the late 1960s, two strains of influenza A virus circulate in the human population. These are known as H1N1 and H3N2. Hemagglutinin (H) and Neuraminidase (N) are two proteins found on the surface of the virus, enabling it to enter cells of the upper respiratory tract. Influenza A viruses are capable of affecting many different species, including birds, pigs, horses and dogs. When viruses from different species mix and infect humans, we typically see pandemics. For example, H1N1, or swine flu, swept the globe in 2009.”
How does the flu vaccine work?
“Historically, the flu vaccine has been what we call a ‘trivalent’ vaccine. This type of vaccine protects us from three different flu viruses: influenza A (H1N1), influenza A (H3N2) and influenza B. It is usually administered as a dead or killed vaccine in which the virus particles are rendered non-infectious, and injected into a muscle in the arm.
“There is also a live virus vaccine – commonly known as ‘FluMist’ – but it has been genetically manipulated, so it can only replicate to a limited extent in the upper respiratory tract. This vaccine does not make you sick. What it does is stimulate very good immunity and antibodies against Hemagglutinin and Neuraminidase, preventing actual infection.
“Last year, a quadrivalent vaccine was introduced. This vaccine protects us against the same viruses as the trivalent vaccine and an additional influenza B virus. By introducing the second influenza B virus, we greatly enhance protection in children and increase vaccine efficacy.”
When should people get vaccinated?
“It is best to receive the vaccine as soon as it becomes available. This usually happens in October or early November.”
Can I get the flu from the vaccine?
“No. You cannot get the flu from the vaccine. In order for the flu to make you sick, the virus needs to get into the lungs. The virus in the vaccine cannot do that. The virus in the flu shot is dead, and the virus in the live-attenuated vaccine cannot get to the lungs.”
How effective is the flu vaccine?
“Vaccine efficacy varies from year to year and among age groups. Some people – the very young and the elderly, for example – simply do not respond to vaccines as well as healthy adults.
“The other thing that can massively affect vaccine efficacy is the closeness to which the strains in the vaccine match the strains that are actually circulating. If the strains that are circulating are a near, or exact, match to the strains incorporated into the vaccine, then the vaccine can provide excellent protection.
“Last year, the main flu that was circulating in adults was a strain of H3N2, and this strain looked very different from the strain incorporated into the vaccine. We call this vaccine mismatch. Essentially, this is a case of bad luck. However, despite this, the vaccine can still provide a limited amount of protection.”
What are the benefits of receiving the flu vaccine?
“There are two major benefits. The first being self-protection. Because influenza is a respiratory illness, a lot of people assume it is just like getting the common cold. This is not true. The problem is that some of the symptoms are similar – a cough or sore throat, for example – but the common cold is much less severe than an influenza virus infection. You will be able to function relatively well with a cold, but the flu can put you out for seven to 10 days.
“The second benefit is the protection of others, particularly at-risk populations. These people include the very young, the very old, those receiving chemotherapy, or on immunosuppressive drugs. If you do not get vaccinated, and become infected with the flu virus, you run the very real risk of passing it onto these people. In some cases, this can be deadly. This concept is known as ‘herd immunity’, and a breakdown in herd immunity can lead to outbreaks. Unfortunately, outside of medical circles, we do not discuss this concept with the public well enough.”
Can you foresee a vaccine that will protect us from all strains of flu?
“We certainly hope so. We, and many others, have been working on a vaccine like this for about five years now, and clinical trials are slated to start in the U.S. at the end of this year. This type of vaccine has worked really well in the lab setting, and we remain hopeful that within the next five to seven years we will see a universal flu vaccine in the marketplace.”